Ref: Diabetes Care 2022;45:1428–1437 | https://doi.org/10.2337/dc21-1957
Introduction
The incidence of unique form of diabetes among individuals with low body mass index (BMI; <19 kg/m2) has been long recognized. Formally classified as “malnutrition-related diabetes mellitus” (MRDM) by the World Health Organization (WHO), this form of diabetes has a high prevalence in low- and middle-income countries (LMICs). The WHO withdrew the MRDM category from diabetes classification in 1999, nevertheless; a substantial amount of data continued to support this unique and fairly prevalent form of diabetes. A correct assessment of patients’ metabolic defects may aid clinicians to appropriately tailor the clinical management in such patients.
Aim
To define the metabolic characteristics of individuals affected with MRDM
Patients Profile
- Patients with lower socioeconomic status (SES) and low BMI (BMI up to 19.5 kg/m2) (n=73)
- All patients were males (age; 19–45 years) with diabetes duration of at least 1 year and having moderate glycemic control (HbA1c 8–10%) and without micro- or macrovascular complications.
- Patients with “low BMI diabetes” (LD; n=20) in whom all forms of diabetes were excluded, were compared with demographically matched groups of patients with type 1 diabetes mellitus (T1DM; n=15), type 2 diabetes mellitus (T2DM; n=13), and a group of individuals without diabetes (lean non-DM; n=16, overweight non-DM; 9).
Results
- Individuals in the LD group had a lower total insulin secretory response as compared with the lean non-DM and the T2DM group.
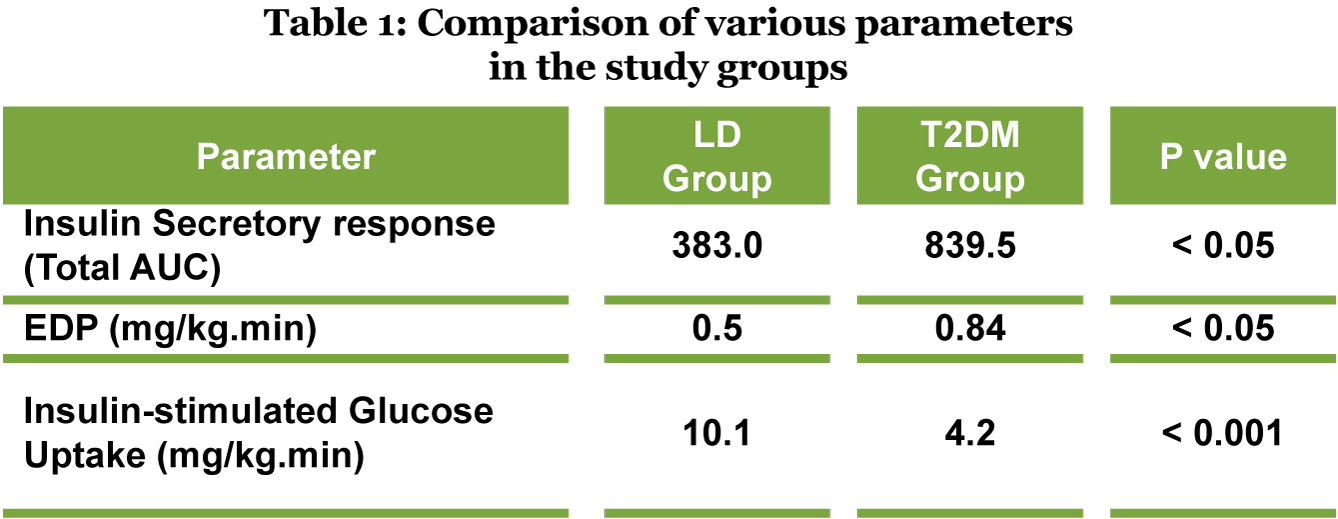
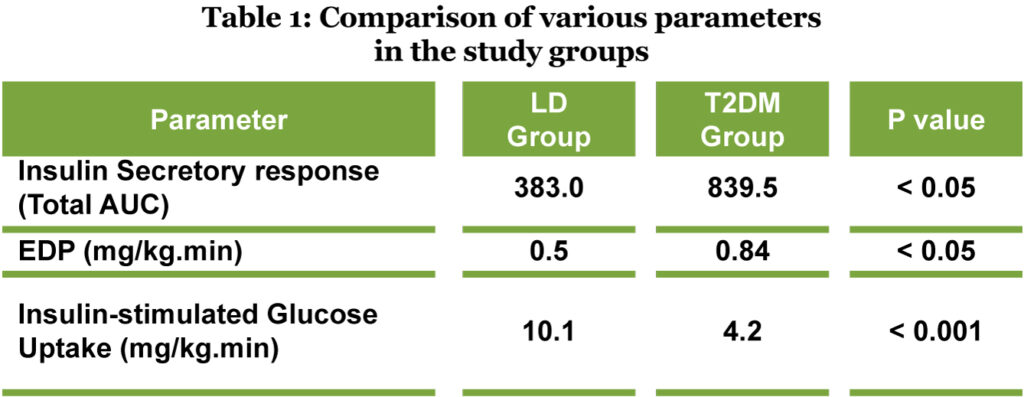
- Individuals in the LD group also had significantly lower endogenous glucose production (EDP) when compared with patients in the T2DM group (Table 1).
- Individuals in the LD group had a significantly higher insulin-stimulated glucose uptake as compared with the patients in the T2DM group (Rd, peripheral insulin sensitivity), suggesting lower peripheral insulin resistance (Table 1).
- Individuals in the LD group had a significantly higher insulin resistance, as compared with the lean non-DM group. Individuals in the LD group also had significantly higher glucose levels at all time points as compared with the lean non-DM group.
- Patients in the LD groups also had significantly lower visceral adipose tissue and hepatocellular lipids as compared with patients in the T2DM group.
Conclusions
- This was a first-of-its kind study that comprehensively characterized insulin secretion, hepatic and peripheral insulin sensitivity, whole body composition, etc. in individuals with LD.
- The study demonstrated that the cardinal physiologic feature of LD was a defect in insulin secretory capacity as opposed to insulin resistance.
- Individuals from LMICs with LD had a unique metabolic profile, suggesting towards a distinct entity that warrants further investigation.