Adapted from Endocrine Today ByErin T. Welsh, MA, Oct-19, 2022
Use of continuous glucose monitoring among children and young adults with type 1 diabetes nearly doubled from 2017 to 2020 in the U.S. from 25% to 49% and was associated with lower HbA1c for users vs. non-users, according to registry data. The rate of CGM use among U.S. residents younger than 25 years remained less than that of their European peers, who saw an increase in use from 40% to 76% during the same period.
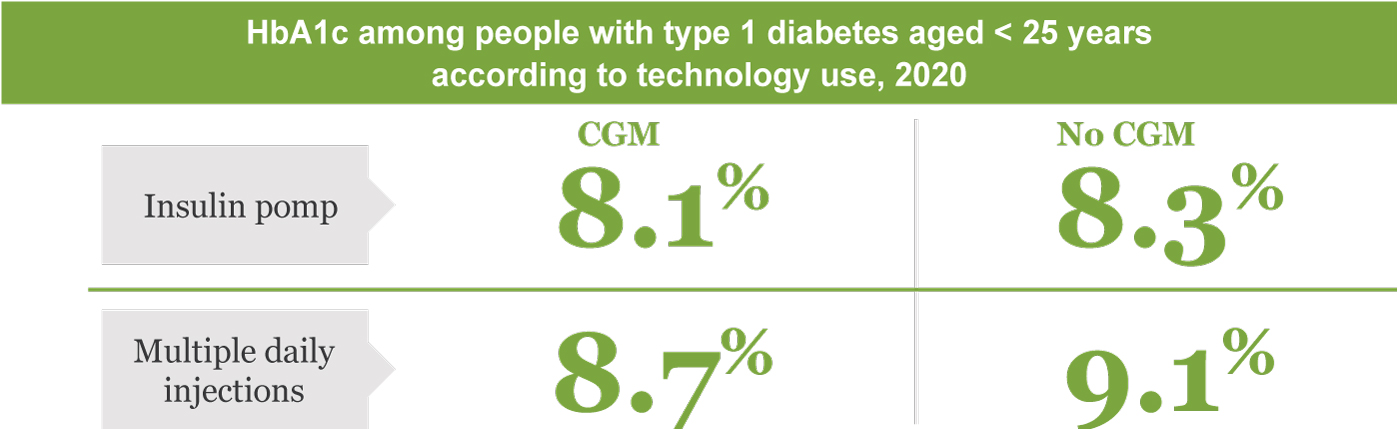
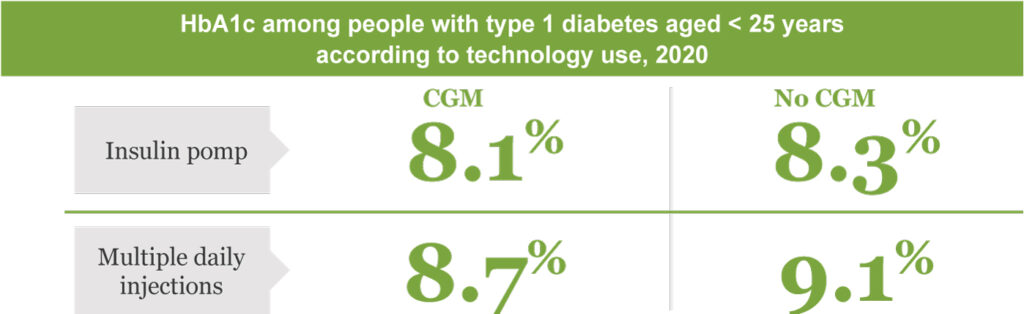
People aged less than 25 years using CGM in 2020 had lower HbA1c than those who didn’t use CGM. Data were derived from DeSalvo DJ, et al. Diabetes Technol Ther. 2022;doi:10.1089/dia.2022.0248.
“Clinical trials provide evidence that CGM improves glucose control and quality of life for children, adolescents and young adults,” Daniel J. DeSalvo, MD, director of strategic collaboration in the division of pediatric diabetes and endocrinology at Baylor College of Medicine at Texas Children’s Hospital, Houston, and colleagues wrote in Diabetes Technology & Therapeutics. “However, even as uptake of CGM in diabetes management is increasing, clinical outcomes vary.”
From 2017 to 2020, across all age ranges, use of CGM increased each year in both European and U.S. registries. In the U.S., use increased for those aged younger than 6 years from 34% to 55%; those aged 6 to younger than 12 years, from 29% to 51%; those aged 12 to younger than 18 years, from 22% to 43%; and those aged 18 to younger than 25 years, from 26% to 46%. CGM use in Europe was greater than that in the U.S. in all age groups in all years except for the18 to younger than 25 years age group in which use increased from 23% in 2017 to 58% in 2020.
Lower mean HbA1c was observed among CGM users younger than 25 years compared with nonusers regardless of the insulin delivery method used for all years (P < .001 for all). During 2020, mean HbA1c was 8.1% vs. 8.3% among users of an insulin pump with vs. without CGM, respectively, in the U.S., and 7.7% vs. 8%, respectively in Europe. Mean HbA1c was 8.7% vs. 9.1% for those using multiple daily injections with vs. without CGM, respectively, in the U.S., and 7.6% vs. 7.9%, respectively, for those in Europe. According to the researchers, these findings are similar to those observed in previous studies of real-world evidence of the steady increase of CGM use and the association of lower HbA1c compared with nonusers in youths with type 1 diabetes.